Dry eye disease : overview and treatment
What is Dry Eye Disease?
Dry eye is complex condition where the eye’s tear film becomes unstable, causing symptoms like discomfort, visual problems, and potential damage to the eye surface. This instability is often due to a combination of factors, including insufficient tear production or poor tear quality, leading to faster evaporation.
Additionally, inflammation and problems with the eye’s sensory nerves can contribute to the disease, making it harder for the eye to maintain a healthy, balanced tear film.
Symptoms
Dryness or Grittiness: A feeling of dryness or something gritty in the eyes.
Redness and Irritation: Eyes may appear red and feel inflamed.
Burning or Stinging: A burning sensation, often worsened by wind or smoke.
Excessive Tearing: Paradoxically, the eyes may water too much due to irritation.
Blurred Vision: Vision may fluctuate or become blurry due to an unstable tear film.
Light Sensitivity: Increased sensitivity to bright light (photophobia).
Eye Fatigue: Eyes tire easily, especially during prolonged tasks like reading.
Foreign Body Sensation: Feeling like something is in the eye, even when it’s not.
Causes
Dry eye is a multifactorial condition with several underlying causes, including:
Tear Film Instability: The tear film, which protects and nourishes the eye, can become unstable due to poor tear production or excessive evaporation. This instability disrupts the balance of moisture, leading to dry eye symptoms.
Meibomian Gland Dysfunction (MGD): The Meibomian glands, located in the eyelids, produce the oily layer of the tear film that slows down evaporation. Dysfunction of these glands is a major cause of Evaporative Dry Eye, as insufficient oil production allows tears to evaporate too quickly.
Reduced Tear Production: In Aqueous Deficient Dry Eye, the lacrimal glands produce fewer tears than necessary. This can occur due to aging, autoimmune conditions like Sjögren’s syndrome, or damage to the glands from inflammation or other factors.
Inflammation: Chronic inflammation plays a central role in dry eye disease. It can damage the tear-producing glands, disrupt the tear film, and cause further irritation and redness, perpetuating the cycle of dry eye symptoms.
Environmental and Lifestyle Factors: External factors, such as exposure to dry air, prolonged screen time, contact lens wear, and certain medications, can exacerbate dry eye by either reducing tear production or increasing evaporation.
Treatments
First-Line Treatments
For those with mild dry eye symptoms, initial management focuses on simple, non-invasive options:
Lifestyle modifications: Improving environmental conditions (such as using humidifiers, taking breaks from screens, and avoiding exposure to wind or smoke) can help alleviate symptoms.
Preservative free lubricant eye drops.
Eyelid hygiene and warm compresses
Omega-3 supplements: Omega-3 fatty acids may help improve the function of the Meibomian glands and reduce ocular surface inflammation.
Second-Line Treatments
When symptoms persist despite initial measures, your eye care provider may recommend:
Prescription anti-inflammatory drops: Medications like cyclosporine (restatis, cequa, Ikervis) or lifitegrast (Xiidra) can reduce inflammation and promote better tear production.
Short-term corticosteroids: These may be used to control acute inflammation.
Punctal plugs: Small devices inserted into the tear ducts to prevent tears from draining too quickly, keeping the eye surface moist for a longer period.
Moisture goggles: Special eyewear designed to protect the eyes from evaporation.
In-office Meibomian gland expression: This involves using heat and pressure to unblock the Meibomian glands to improve tear stability, which can be performed manually or with devices like LipiFlow.
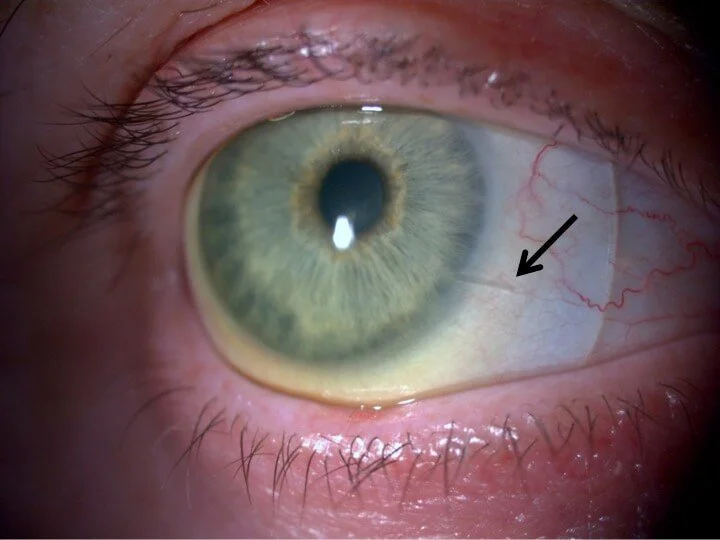
Intense Pulsed Light (IPL) therapy: Primarily used for patients with Meibomian Gland Dysfunction, IPL has been shown to reduce inflammation and improve gland function.
Advanced Interventions
For patients with moderate to severe dry eye, more advanced treatments may be necessary:
Scleral contact lenses Scleral contact lenses improve dry eye by creating a fluid reservoir between the lens and the eye, which keeps the corneal surface hydrated and protects it from environmental irritants.
Autologous serum eye drops: These are eye drops made from the patient’s own blood and contain essential growth factors that help repair the eye’s surface and stabilize the tear film.
Oral antibiotics - doxycyline : taken to reduce inflammation and improve the function of the oil glands in the lids.
Permanent punctal occlusion: Surgically blocking the tear ducts to prevent tears from draining.
Silicone punctal plug for dry eye
scleral lenses can protect the eye surface in severe dry eye
FAQs
Can dry eye be cured?
Dry eye cannot usually be cured, but it can be managed effectively with proper treatment. Symptoms can often be controlled with artificial tears, prescription medications, lifestyle changes, and, in severe cases, procedures like punctal plugs or scleral lenses.
Is dry eye related to age?
Yes, dry eye is often related to aging. Tear production tends to decrease as we age, particularly in people over 50, and hormonal changes during menopause can also contribute to dry eye in women.
Is dry eye related to computer use?
Yes, prolonged computer use is a common trigger for dry eye symptoms. People tend to blink less frequently when staring at screens, which reduces tear distribution and increases eye dryness.
Can dry eye lead to blindness?
While dry eye itself does not typically lead to blindness, severe and untreated dry eye can cause damage to the cornea, leading to scarring or infection, which can impair vision. Proper management of dry eye helps prevent these complications.
What are the best eye drops for dry eyes?
First-line treatments for dry eye includes preservative free over the counter lubricant drops, such as Hyloforte, Hylofresh, Systane Hydration UD, Theratears, Cationorm. Gel or ointments- such as Theratears Gel, Vitapos, and Celluvisc are formulated to provide better contact time overnight. Your optometrist may prescribe medicated eye drops for more severe cases of dry eye.
Can dehydration lead to dry eye?
Hydration is important for maintaining healthy tear production and eye moisture. Dehydration can worsen dry eye symptoms by reducing tear production and affecting tear quality, so staying well-hydrated helps keep the eyes properly lubricated.
Can certain medications worsen dry eye?
Several medications, including antihistamines, beta-blockers, diuretics, and antidepressants, can lead to dry eyes by reducing tear production or affecting tear composition. Hormone replacement therapy, oral contraceptives, and medications like Accutane or those for Parkinson's disease can also contribute to dry eye symptoms.
Is IPL for dry eye safe?
Intense Pulsed Light (IPL) therapy for dry eye disease is generally regarded as safe, with minimal and temporary side effects. The most common side effects include mild discomfort, redness, and a burning sensation, all of which typically resolve quickly. IPL is particularly effective for meibomian gland dysfunction-related dry eye and reduces inflammation by targeting dilated blood vessels. However, care must be taken to protect the eyes during treatment to avoid damage, and IPL may pose a higher risk of pigmentation changes in individuals with darker skin types. While it is a promising therapy, further long-term studies are needed to fully assess its safety across different populations and skin types.
Conclusion
Dry eye disease is complex and can differ significantly between patients- dry eye treatment often targets different aspects of the disease and needs to be highly individualised. Mild cases of dry eye can be treated with environmental modification and optometrists may prescribe at home treatment regimes. More advanced cases may require prescription medication and / or additional in-office treatments such as IPL, punctal plugs, and in-office meibomian expression.
In our clinic, we can offer advanced management of dry eye, including medical management, IPL, punctal plug fitting, in-office meibomian expression, and scleral contact lenses.
References
Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS II):
Willcox, M.D.P., et al. "TFOS DEWS II Tear Film Report." Ocular Surface, 2017. Link to TFOS DEWS II.
A Review on Dry Eye Disease Treatment: Recent Progress, Diagnostics, and Future Perspectives:
Mondal, H., Kim, H., & Jee, J.P. "A Review on Dry Eye Disease Treatment: Recent Progress, Diagnostics, and Future Perspectives." Pharmaceutics, 2023. Link to the article(
Advances in the Pathophysiology, Diagnosis, and Treatment of Dry Eye Disease:
Editorial. "Advances in the Pathophysiology, Diagnosis, and Treatment of Dry Eye Disease." Frontiers in Ophthalmology, 2021. Link to the article(
Author Bio
Jenny Wu is an optometrist based in Canberra, Australia. She is a full scope optometrist specializing in dry eye, specialty contact lenses, myopia control, and orthok. She practices at Simpson Optometry. In her spare time she enjoys spending time in nature, photography, gardening, and being with her husband (also an optometrist) and 2 children.